When a person with type II diabetes develops high blood sugar levels (hyperglycemia), they may experience symptoms such as excessive thirst, frequent urination, increased appetite, weight loss, blurred vision, fatigue, headaches, occasional muscle cramps and poor wound healing. However, there are a lot of people with type II diabetes who do not show symptoms and don't even know they have it.
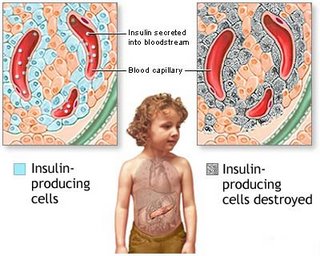
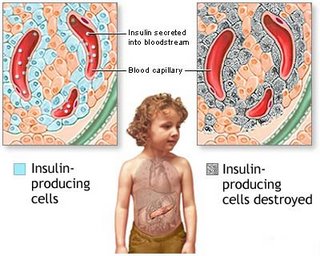
In type I diabetes, however, the symptoms occur more abruptly, progressing to a potentially life-threatening condition called diabetic ketoacidosis (DKA). DKA is unique to type I diabetes. When insulin is lacking, the glucose is not able to enter the cells and blood sugars rise dramatically. Symptoms are excessive thirst, frequent urination, weight loss, nausea, vomiting, and fatigue. DKA could lead to coma and death if treatment is not given to lower blood sugars.
What are the complications of diabetes?There are several complications that can arise as a result of poorly controlled diabetes.
1. Macrovascular Disease
• Coronary Artery Disease — Many studies have revealed that coronary artery disease accounts for over 50% of all deaths in patients with diabetes. Some studies have shown that insulin resistance, such as in type II diabetes, may be associated with atherosclerosis.
• Hypertension — is almost twice as common in people with diabetes than nondiabetic individuals.
• Cerebrovascular Disease — affects the vessels leading to the brain. Blockage of one of the major cerebral vessels causes a stroke due to a lack of oxygen to the brain. Cerebrovascular disease seems to develop at an earlier age in people with diabetes. Mortality rates are from three to five times greater than those who do not have diabetes.
• Peripheral Vascular Disease (PVD) — is very common in people with diabetes. PVD is similar to cardiovascular disease, but it affects the vessels in the lower extremities of the body such as the legs. As the arteries are narrowed, less blood and oxygen is delivered to the extremities. The legs feel achy, fatigued and painful. The feet may become numb and cold, the skin dry and scaly. A person may develop sores that are difficult to heal. A complete obstruction of blood supply can lead to gangrene (tissue death).
2. Retinopathy — occurs when the small vessels that nourish the retina portion of the eye are damaged. This causes a leakage of blood components through the vessel walls. The retina allows for the focusing of images and light.
3. Neuropathy — Diabetic neuropathy is a condition in which nerve fibers are damaged. The cause is related to either insulin deficiency and/or high blood sugars. Diabetic neuropathy can cause disruptions in sensations, muscle activity and the function of internal organs. The person may experience tingling, pain, numbness, and even burning sensations in various parts of the body such as the feet and hands. If no pain is felt, they may burn themselves or develop sores from prolonged pressure. Other areas of the nervous system could be affected that regulate blood pressure, bowel and bladder control and heart rhythm.
4. Nephropathy — Diabetic nephropathy is a type of kidney disease in which kidney function declines as a result of multiple factors, including poorly controlled diabetes and/or blood pressure. The kidneys act as a filter, removing waste products from the blood and eliminating them from the body as urine. When kidney function declines, these wastes become toxic to the body as they build up in the bloodstream. Fluid retention becomes massive when the ability to urinate decreases, causing weight gain, fatigue, shortness of breath and uncontrolled blood pressure. Eventually, the kidneys stop working (kidney failure) and people become dependent on dialysis machines to filter their blood.
 - Nausea and vomiting. It is common to experience nausea and vomiting during the first trimester. Although this condition is often referred to as morning sickness, it can occur at any time of day. It is most likely the result of pregnancy hormones relaxing the stomach muscles. Women may benefit from eating frequent, small meals and drinking a lot of liquids. Nausea and vomiting usually disappear after the first trimester. Women who are vomiting a lot, or vomiting with pain or fever should immediately contact their ObGyn (see Morning Sickness).
- Nausea and vomiting. It is common to experience nausea and vomiting during the first trimester. Although this condition is often referred to as morning sickness, it can occur at any time of day. It is most likely the result of pregnancy hormones relaxing the stomach muscles. Women may benefit from eating frequent, small meals and drinking a lot of liquids. Nausea and vomiting usually disappear after the first trimester. Women who are vomiting a lot, or vomiting with pain or fever should immediately contact their ObGyn (see Morning Sickness).  - Frequent urination. Many woman need to urinate more often during early pregnancy. This is the result of the uterus pressing on the bladder as it grows. This pressure may also cause a woman to leak urine while sneezing, coughing or laughing (incontinence). Women experiencing pain or burning during urination, and those who notice pus or blood in the urine, should contact their ObGyn. This may indicate a urinary tract infection
- Frequent urination. Many woman need to urinate more often during early pregnancy. This is the result of the uterus pressing on the bladder as it grows. This pressure may also cause a woman to leak urine while sneezing, coughing or laughing (incontinence). Women experiencing pain or burning during urination, and those who notice pus or blood in the urine, should contact their ObGyn. This may indicate a urinary tract infection